Bengaluru: Genetic diagnostic and drug discovery research firm MedGeneome Labs Thursday claimed to have developed the first whole genomic sequencing-based test to detect drug-resistant mutation in tuberculosis (TB) bacteria.
“The breakthrough DNA test will enable a doctor to correctly prescribe the most effective drug to a TB patient without a time-consuming trial and error process,” said the city-based clinical data-driven Labs.
Announcing its foray into infectious disease testing in TB, central nervous system (CNS), systemic and eye infections, the company said India had the largest number of multi-drug resistant (MDR) TB cases.
“India has the largest number of MDR-TB cases. Our spit sequence can be a boon for TB patients, clinicians and healthcare agencies to achieve the sustainable development goal of eliminating TB by 2025,” Labs Chief Operating Officer VL Ramprasad told reporters here.
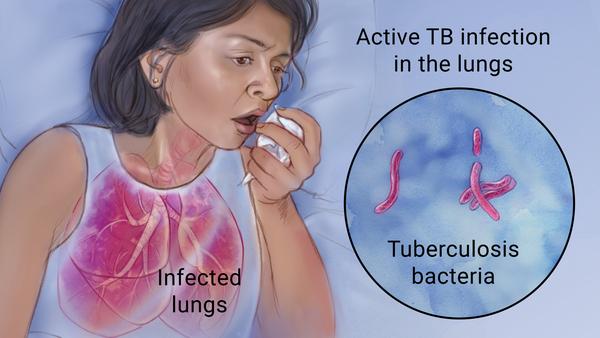
“The test is based on the whole genome sequencing of mycobacterium tuberculosis (MTB), the TB causing bacteria, to assess the mutations in bacteria’s genome and allows a clinician to determine which drug will work for a patient,” he said.
Mumbai-based PD Hinduja Hospital and Medical Research Centre head Camilla Rodrigues said the test was validated with 100 samples recording 100 per cent sensitivity and 98.04 per cent specificity compared with line probe assay technology.
“Of the 100 samples, 50 were tested in our hospital. The findings in the manuscript are under review for publication,” Rodrigues said on the occasion.
Noting that the process of analyzing the drug resistance was long, which is delaying early treatment for MDR-TB patient, Rodrigues said the current expertise allowed testing resistance only on 4 drugs, which makes the patient wait until testing on all possible drugs concluded.
“Direct whole genome sequencing reveals information on drug resistance mutations for all anti-TB drugs in 10 days. Our testing will help to optimise the management of an MDR-TB patient”, she added.
(IANS)