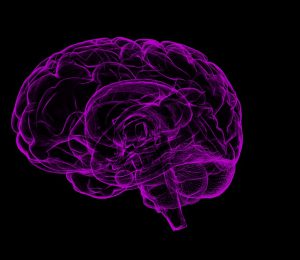
New Delhi: Scientists have developed a new 3D printing technique that they say could provide tailored repairs for those who suffer brain injuries.
The researchers at the University of Oxford in the UK demonstrated for the first time that neural cells can be 3D printed to mimic the architecture of the cerebral cortex, the outer layer of the human brain.
Brain injuries, including those caused by trauma, stroke, and surgery for brain tumours, typically result in significant damage to the cerebral cortex, leading to difficulties in cognition, movement, and communication.
The researchers noted that each year, around 70 million people globally suffer from traumatic brain injury (TBI), with 5 million of these cases being severe or fatal.
Tissue regenerative therapies, especially those in which patients are given implants derived from their own stem cells, could be a promising route to treat brain injuries in the future, the researchers said.
However, till now there has been no method to ensure that implanted stem cells mimic the architecture of the brain, they said.
In the study published in the journal Nature Communications, the researchers fabricated a two-layered brain tissue by 3D printing human neural stem cells.
When implanted into mouse brain slices, the cells showed convincing structural and functional integration with the host tissue, they found.
“This advance marks a significant step towards the fabrication of materials with the full structure and function of natural brain tissues,” said study lead author, Yongcheng Jin, from the Department of Chemistry, University of Oxford.
“The work will provide a unique opportunity to explore the workings of the human cortex and, in the long term, it will offer hope to individuals who sustain brain injuries,” Jin said.
The cortical structure was made from human induced pluripotent stem cells (hiPSCs), which have the potential to produce the cell types found in most human tissues.
A key advantage of using hiPSCs for tissue repair is that they can be easily derived from cells harvested from patients themselves, and therefore would not trigger an immune response.
The hiPSCs were differentiated into neural progenitor cells for two different layers of the cerebral cortex, by using specific combinations of growth factors and chemicals. The cells were then suspended in solution to generate two ‘bioinks’, which were then printed to produce a two-layered structure.
In culture, the printed tissues maintained their layered cellular architecture for weeks, as indicated by the expression of layer-specific biomarkers.
When the printed tissues were implanted into mouse brain slices, they showed strong integration, as demonstrated by the projection of neural processes and the migration of neurons across the implant-host boundary, the researchers said.
The implanted cells also showed signalling activity, which correlated with that of the host cells, indicating that the human and mouse cells were communicating with each other, demonstrating functional as well as structural integration, they said.
The researchers said they now intend to further refine the droplet printing technique to create complex multi-layered cerebral cortex tissues that more realistically mimic the human brain’s architecture.
Besides their potential for repairing brain injuries, these engineered tissues might be used in drug evaluation, studies of brain development, and to improve our understanding of the basis of cognition, they added.
PTI